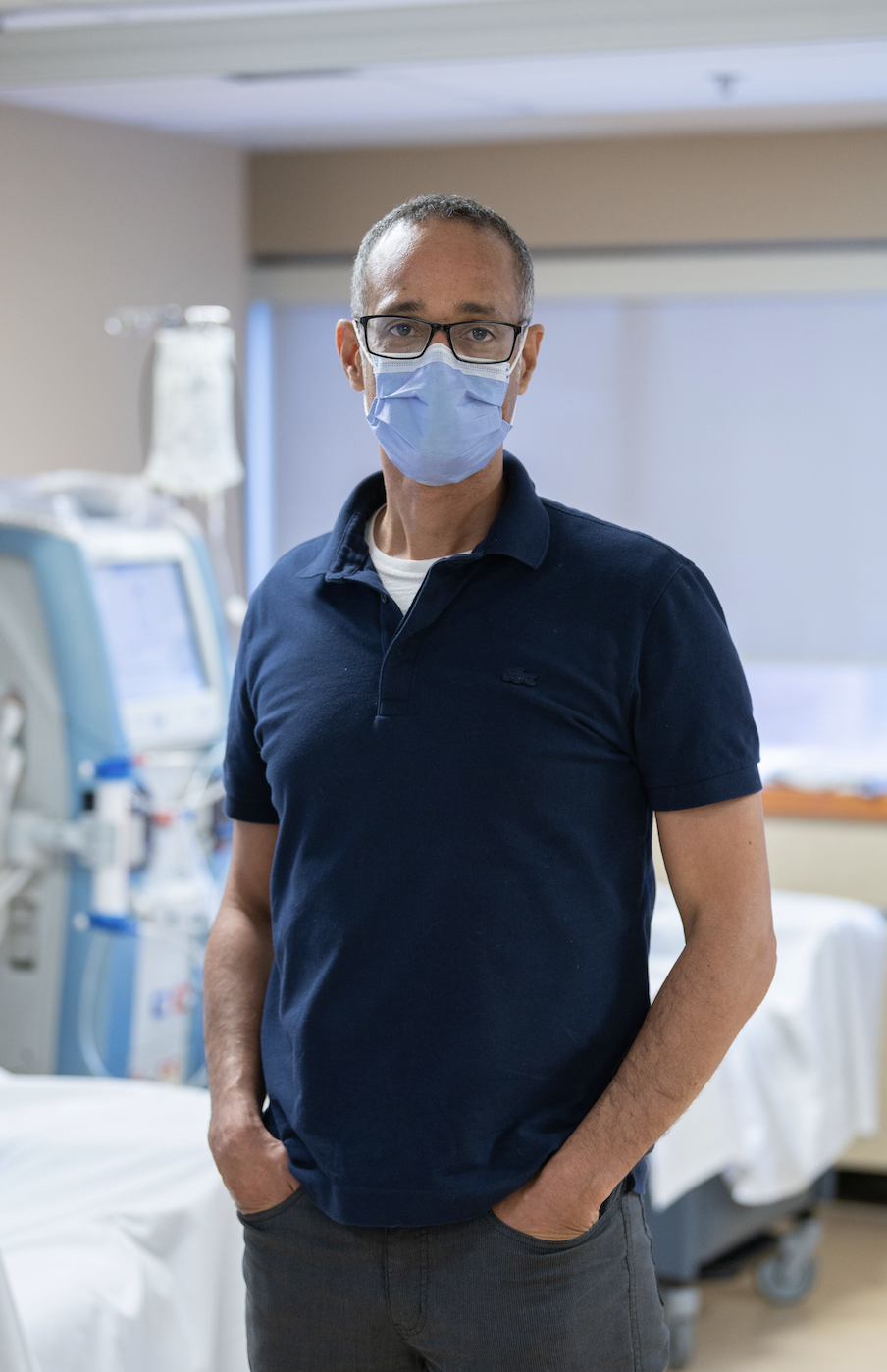
 Described by his patients as “approachable, kind, and knowledgeable,” Dr. Tabo Sikaneta is well-loved throughout the community. As a nephrologist, Dr. Sikaneta works in the kidney unit at Scarborough Health Network (SHN), dealing primarily with dialysis and inpatient kidney care.
Described by his patients as “approachable, kind, and knowledgeable,” Dr. Tabo Sikaneta is well-loved throughout the community. As a nephrologist, Dr. Sikaneta works in the kidney unit at Scarborough Health Network (SHN), dealing primarily with dialysis and inpatient kidney care.
Dr. Sikaneta explains the importance of the life-sustaining nephrology program even during a pandemic, along with a personal reflection on his journey working in kidney care for 19 years.
Editor’s Note: This interview has been edited for length and clarity.
How did COVID-19 impact the nephrology program?
At SHN, it was important that nephrology services, particularly when it came to the provision of hemodialysis, be maintained throughout the pandemic. When kidneys fail completely, a person is dependent on a kidney transplant or dialysis treatments to stay alive. Patients on hemodialysis need their treatment two or usually three days a week to keep going.
So the nephrology program wasn’t as affected as other areas within the hospital. Pandemic or no pandemic, our patients had to continue coming to hospital for their lifesaving treatments. Also, when complications arose that needed to be addressed in hospital, like infections or heart disease, our patients were still admitted.
What did change, of course, was that we had to care for kidney patients with COVID-19. Dialysis patients are more susceptible to getting very sick from COVID-19, and some other patients – who had no previous kidney problems – developed kidney failure because of COVID-19. So, in the intensive care unit (ICU) especially, we saw more new cases of kidney failure.
What is it like wearing Personal Protective Gear, such N95s, gowns, and face shields, all-day long?
It was quite trying. It was challenging to interact with other staff and patients because of all of the layers of protective gear and the need to ensure physical distancing. Due to the sheer volumes of our patients, there was a lot of donning and discarding of protective gear, and then there was always the concern that despite this we were still at risk of exposure when working with confirmed cases of COVID-19.
It was very uncertain for a lot of people when the pandemic first started. How did you and your team support each other during those challenging times?
It was a scary time. There was a lot of fear as no one really knew what was going to happen or how much worse things were going to get. When the first few patients came down with COVID, we didn’t know what was going to happen to them, how much this was going to spread within the dialysis population, or to us as the dialysis care providers and therefore to our families at home.
We made some changes to our hospital schedules so that we could have clear “on’ and “off’ times when it came to our provision of care to inpatients. During the “on’ times when we were in the trenches so to speak, some of the staff members would take up separate residences, or separate themselves from other family members within their homes.
How was the nephrology program handling COVID-19 vaccine in patients?
We believed early on that vaccination would be a powerful way to protect our patients, and we were one of the most proactive units – not just within the hospital but among dialysis units around the province – in getting our patients vaccinated. We were able to get our patients prioritized for the vaccines, and marshalled the resources – including the staff that worked tirelessly around the clock – to get them vaccinated. It was quite an undertaking, and this credit is due to Dr. Paul Tam the Program Director, and the team of nurse managers and nurses, as well as our Senior Leadership Team who all helped to make this happen.
What is the most important quality of the care experience for kidney patients?
Trust. They must trust their doctors and health care team because they are very vulnerable patients who put themselves in very compromised positions week in and week out. At each treatment our hemodialysis patients are connected to machines that pull out all their blood to clean it, and are at risk for all manner of problems – including blood pressure changes, vomiting, cramps, adverse reactions, infections, heart problems just to name a few. Kidney patients therefore have to be able to trust their lives with us.
Another important quality is that they feel their wishes are respected. Kidney failure and dependence on dialysis already represents the loss of so much control over one’s health, and it is critical to remember and respect the dignity and wishes of patients.
Have you noticed any changes or trends in what types of patients are coming into the hospital?
I’ve worked at the hospital since 2003, and the relentless growth of the program has been quite striking. At 7 per cent, the annual rate of growth is double the provincial average. I have also been struck by the disparities apparent in people who get kidney failure, especially among subgroups of people who were not born in Canada and people of non-White ethnicities. Given that Scarborough is already so diverse and growing so rapidly, it is perhaps no wonder that the program is growing so fast. What is a wonder is the opportunity presented to better understand who gets kidney disease and why here in Scarborough, and the challenge to buck this trend.
What do you enjoy about your job?
I love nephrology because you develop long-term relationships with your patients. You have a lot of patient contact. They get to know you and trust you, and vice versa. Similarly, I enjoy working with and developing long-term relationships with my colleagues and other kidney health care professionals. In many ways we are like a family.
I love the fact that it’s challenging, cerebrally. It requires you to have one foot in general internal medicine and another foot in the speciality aspects of it, like dialysis.
I love the opportunity to make a meaningful impact in those patients who have reversable or treatable kidney disease. When that happens nephrology can be very rewarding.
I also love the breadth of practice. We care for inpatients in all departments throughout the hospital, and see outpatients in a variety of clinics. There’s also a strong bend to primary care prevention, for example by preventing or treating diabetes or high blood pressure – the main causes of kidney disease.
Anything else you would like to add?
Scarborough is a fantastic place to work as a nephrologist! Pulling together to get the job done during a global pandemic demonstrated how strong is the teamwork ethic of SHN’s regional kidney program. The sheer volume and pace of growth of kidney disease, also means that working in Scarborough offers many other opportunities to make a difference, not just for patients here and now, but for patients elsewhere and in the future. I believe there are secrets and lessons of nephrology right here in Scarborough to seek and broadcast beyond its borders!